In southern China, there’s a notorious “villain” obsessed with people from the south. It displays strong regional discrimination, mainly targeting those from Guangdong, Guangxi, Hunan, Fujian, Jiangxi, Hainan, and Hong Kong–Macau areas. It’s called nasopharyngeal carcinoma (NPC), also known as the “Cantonese Cancer.” Mr. Zhang (pseudonym) from Hong Kong became one of its latest targets.
“In my left ear, I kept hearing ringing and couldn’t hear clearly. There was always blood in my nasal discharge...” In 2022, Mr. Zhang was diagnosed with a mass in his nasopharynx. A biopsy confirmed it as a malignant tumor. The local hospital recommended chemotherapy and radiotherapy, but he refused without hesitation. Many of his friends had been through similar experiences and warned him that radiotherapy not only requires tooth extraction beforehand but also brings lifelong side effects. The treatment process is so painful that it drove some patients to suicidal thoughts.
As a result, Mr. Zhang chose traditional Chinese medicine, but his symptoms did not improve. In 2024, he traveled to Japan in hopes of trying cellular immunotherapy. However, after eight months, there was no improvement. Worse still, the tumor in his neck had grown to the size of a tennis ball. He was suffering from difficulty opening his mouth, shortness of breath, headaches, and hearing loss—all of which severely tormented him.
“Go to Fuda Cancer Hospital in Guangzhou!” Mr. Zhang recalled a report about Fuda successfully treating nasopharyngeal carcinoma. After speaking with hospital staff, he made a decisive move and sought care at Fuda Medical Center’s Department III (Head and Neck Oncology) in March 2025.
Mr. Zhang’s condition upon admission was dire: the tumor in his neck was massive, at risk of rupture at any time, posing an imminent threat to his life. His wife was extremely anxious. Understanding the urgency, Director Xu Jiongyuan of Department III prioritized tumor control and symptom relief.

△ Condition upon admission
Further examination revealed that the tumor had invaded the skull base, intracranial brain tissue, oropharynx, and bilateral cervical lymph nodes. After a multidisciplinary discussion and evaluation, considering the tumor’s large size and rich blood supply, an individualized interventional treatment plan was developed.
The first step was arterial infusion chemotherapy targeted at the nasopharyngeal lesion. Given Mr. Zhang’s poor general condition at admission, the treatment was carried out using low-dose chemotherapy to minimize adverse effects. After this round of chemotherapy, imaging showed tumor shrinkage, indicating that the treatment was effective.
Next, using super-selective catheterization, arterial infusion chemotherapy combined with chemoembolization was performed. This involved precisely delivering drugs into the tumor core and then injecting embolic agents to block the tumor’s blood supply. This approach cut off the tumor’s nutrient source while protecting healthy surrounding tissues, enabling a high concentration of medication to act directly on the tumor.

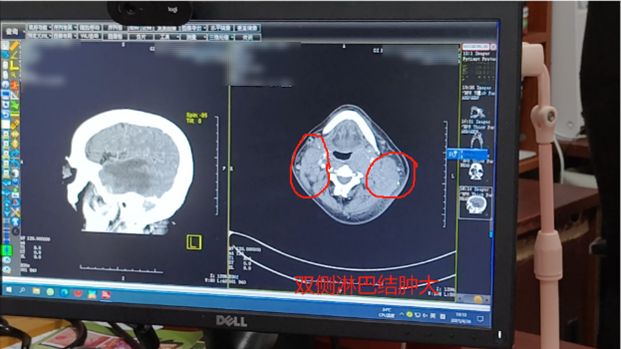
Post-treatment imaging showed significant tumor shrinkage on both sides.
“I could clearly feel the tumor in my neck shrinking—it's amazing,” said Mr. Zhang. Both he and his wife were astonished by the results and delighted by the symptom relief. After two rounds of interventional treatment, follow-up examinations showed that the bilateral masses had reduced from 10×8 cm and 10×9 cm to 4×5 cm and 5×6 cm. Redness and swelling subsided significantly. Tumor markers such as CEA and SCC antigen also declined. The treatment efficacy was assessed as PR (partial response).
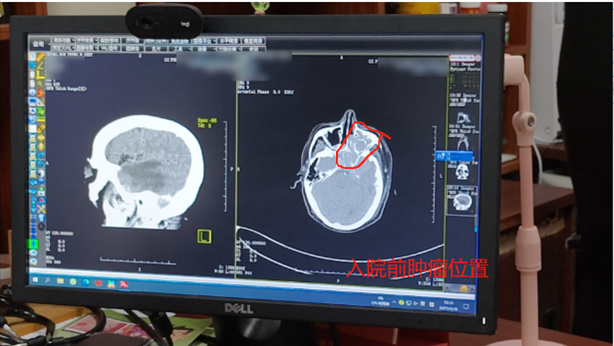
△ Imaging before admission
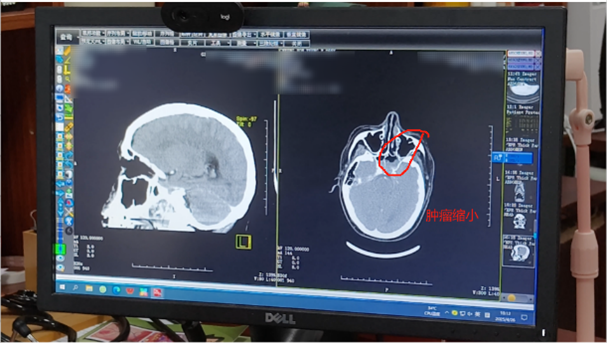
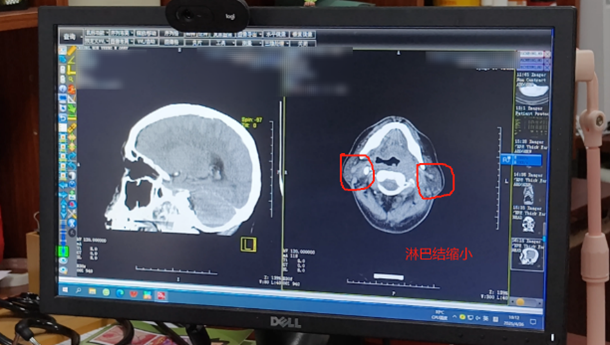
△ Imaging after treatment
“We had mentally prepared for the worst, but thankfully Fuda had multiple technical solutions to offer me a ‘way out’.” Before admission, even painkillers couldn’t relieve Mr. Zhang’s suffering, and he could only consume liquid food. Now, after treatment, the tumor has shrunk, pain is relieved, and he is eating normally. He attributes all of this to Fuda’s advanced medical technology and outstanding healthcare services. “No one wants to be hospitalized, but the staff here are warm and caring, which makes us feel at ease.”
Currently, Mr. Zhang continues to receive interventional treatment and immunotherapy to further control the tumor and create opportunities for curative radiotherapy.

Health Tips
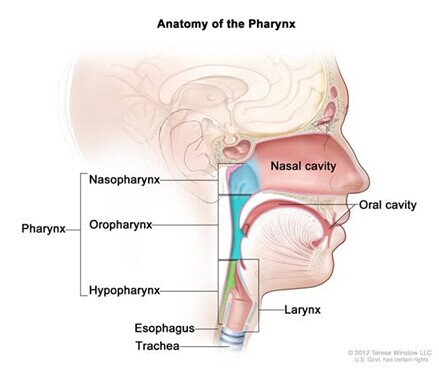
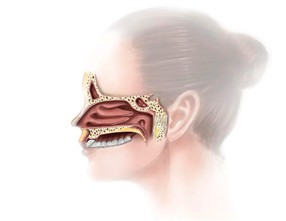
As the name suggests, nasopharyngeal carcinoma (NPC) is a malignant tumor that occurs in the nasopharynx. Because it develops deep within the head and has a hidden onset, early-stage tumors are small and hard to detect. Being adjacent to the eyes, ears, throat, and skull base, it easily invades nearby organs through the submucosa or spreads via the lymphatic system.
NPC is highly malignant and often metastasizes to the cervical lymph nodes even in early stages. Many patients are already in the advanced stages by the time obvious symptoms appear, so early detection of abnormalities is crucial. Classic symptoms include nasal congestion, blood-tinged mucus, tinnitus, hearing loss, headaches, facial numbness, and double vision. Key physical signs include nasopharyngeal masses, cervical lymph node metastasis, and cranial nerve involvement.
Director Xu Jiongyuan emphasizes: If any of these symptoms occur, patients should promptly visit a specialized hospital. Nasal endoscopy often reveals nasopharyngeal masses, and a biopsy can confirm the diagnosis. If nasal endoscopy shows no clear abnormalities but symptoms persist, enhanced MRI or CT scans may be needed. In some cases, a deep tissue biopsy is required for diagnosis.
It’s important to note that symptoms like blood-tinged mucus and ear congestion are not unique to NPC; they can also occur in benign conditions such as otitis media or sudden deafness. So while it’s important to seek medical evaluation promptly, there’s no need for undue panic.